Weight-Bearing Post-Fixation of Pelvic Facture: A Systematic Review
Weight-Bearing Post-Fixation of Pelvic Facture: A Systematic Review.
Introduction
Over the last three decades, pelvic fracture surgery has
noticeably increased worldwide due to the enhancement of healthcare for patients
suffering from traumatic pelvic injury. In Belgium, the overall incidence of
pelvic fractures increased from 15,8/100.000 persons per year in 1988 to
37,6/100.000 persons per year in 2018 (Herteleer et al., 2021). In Sweden, the incidence of
pelvic fractures increased from 64 to 80 per 100,000 person-years from 2001 to
2016 mostly among females (74% of the overall incidence) (Lundin et al., 2021). In a Nordic country, the
incidence of pelvic fracture that requires hospitalization increased from 34 –
56/100,000 person-year from 1997-2014 (Rinne et al., 2020). In France, the Incidence of
pelvic fractures per 100,000 person-years increased from 17.1 in 2006 to 28.33
in 2016 with male predominance (Melhem et al., 2020). By 2030, the number of hip
fracture patients is projected to be nearly 300,000 patients in the USA (Miyamoto et al., 2008). Thus, orthopedic researchers
have been particularly interested in the outcome of interventions to fix pelvic
fractures.
Pelvic fractures are caused by energy force ranging from
low-energy force causing minor or isolated fractures to high-energy force
causing major pelvic ring disruptions (Yoshihara & Yoneoka, 2014). Consequently, the elderly
population is prone to low-energy minor pelvic ring fractures after low-impact
fall (Herteleer et al., 2021) that carries poor outcomes (Ayoung-Chee et al., 2014). Currently, pelvic fractures
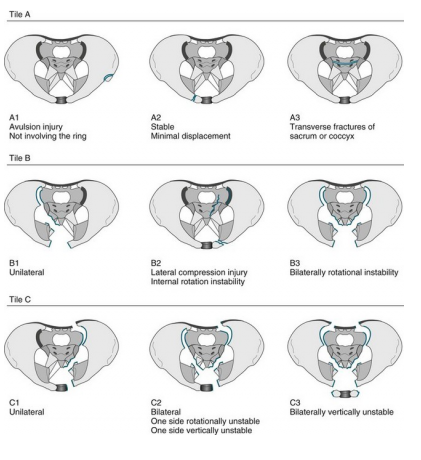
are classified according to Tile system to Type A where the pelvic ring is
stable, Type B which is partially stable including “open-book” and
“bucket-handly” fractures, and Type C with a complete disruption of the
posterior sacroiliac complex (Tile, 1996; Tile & Pennal,
1980).
Moreover, the Young and Burgess classification system depends on computed
tomographic (CT) pictures categorizing pelvic fracture into Lateral compression
(LC), anteroposterior compression (ABC), vertical shear (VS), and combined (Young et al., 1986).
The application of post-fixation weight-bearing in the rehabilitation
of patients who carried out pelvic fracture fixation surgery is a challenging
topic. The current consensus is that no weight-bearing or toe-touch weight-bearing
should be practiced as an early therapeutic approach in patients with unstable
pelvic fractures (Murena et al., 2021). According to the American
Academy of Orthopedic Surgeons (AO), an interval of 10-12 weeks should elapse
before the initial graduation of weight bearing by a 25% increment per week (Roberts et al., 2015). Moreover, for rotationally unstable but
vertically stable pelvic fractures, the recommendation of the British
and Irish surgeon consultants was against early weight-bearing that should be
delayed for 8-12 weeks postoperatively (Gill et al., 2017). The rationale for delaying
weight bearing is based on the empirical knowledge of experts practicing
post-fixation pelvic fracture surgery for years (Kalmet et al., 2018). The main concern is centered
around the reduction of shearing forces at the site of the fracture to promote
bone and ligament healing, reduction of implant failure risk, fear of fracture
displacement, and avoidance of malunion or nonunion (Eickhoff et al., 2022; Paulsson
et al., 2021).
On the other hand, it is theorized that early weight-bearing
of post-fixation pelvic fracture surgery provides valuable benefits including
maintaining bone stock and muscle mass, preserving the range of movement, and
improving rehabilitation as per the patients’ goals (Poole et al., 2022). Moreover, early weight
bearing would minimize the incidence of venous thromboembolism (VTE) (Dwyer & Moed, 2019; Nelson
et al., 2020)
and pulmonary embolism (PE) (Kim et al., 2021) in post-operative bed-ridden
patients. Furthermore, it was concluded that compliance with weight-bearing is
low among the aged population more than 65 years as well as weight-bearing
education (Seo et al., 2020). In addition, early weight
bearing shortens the period to return to work with the reduction of the cost
burden (Kubiak et al., 2013). However, the scientific
evidence base to make recommendations is lacking (Rickman et al., 2019).
To apply unrestricted weight-bearing of post-fixation pelvic
surgery, evidence of the safety and efficacy of the weight-bearing approach
should be established. Loss of reduction that mandates reoperation is the main
concern of the weight-bearing debate. Therefore, the current study reviewed all
post-fixation pelvic fracture surgery patients who carried out the
weight-bearing approach from 2017 to 2022. The main aim of the study was to
assess the safety of the weight-bearing approach. In addition, this review was
carried out to explore the indications for weight-bearing in post-fixation
pelvic fracture surgery to emphasize and detect clinical evidence for practical
recommendations supporting the weight-bearing approach.
Methods
The Preferred
Reporting Items for Systematic reviews and Meta-Analyses (PRISMA)
statement guidelines (Moher et al., 2009) were followed throughout the
processing stages of this study. The processing stages were performed according
to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins, 2003).
Eligibility Criteria
Studies were included according to the following criteria:
(1) adult participants more than 18 years of age suffering from a pelvic
fracture that mandates operative intervention; (2) the study design could be
double arm designs, randomized controlled trials (RCTs), case studies and case
series, clinical trials, and case-control studies; (3) Studies published in
English; (4) studies from 2017-2022; (5) studies focusing on or including rotationally unstable but
vertically stable pelvic fracture (Tile classification: Type B pelvic
fracture); (6) studies that adopt early weight bearing as post-fixation therapy
for a minimum period of 6 months at least.
Moreover, we excluded studies carried out on patients less
than 18 years of age, study designs including conferences, abstracts,
unpublished preprint studies data, editorial letters, and studies written in a
language other than English.
Outcomes
The outcomes were attributed to reported results either
formal outcome scores or descriptive discourse with a minimum follow-up of 6
months. The primary
outcomes were the quality of life and pain within 6 weeks of post-operative
weight-bearing following a pelvic fracture. In addition, post-operative
weight-bearing regimens were recorded and included in the review as a secondary outcome.
No comparison was carried out between the weight-bearing regimen in this study.
Endpoints
The endpoints included the endpoint of the study follow-up.
The follow-up
periods were recorded and reviewed as well.
Search Strategy and Study Selection
Using
relevant keywords, the databases PubMed, Scopus, Cochrane, Web of Science,
Embase, and Science Direct were searched. The recent papers from 2017 to 2022
were identified and selected. The used search terms include “fracture pelvis,”
“pelvic trauma,” pelvic ring fracture,” pelvis fracture,” and “pelvic
fracture.” Other search terms were used to meet the aim of the study including
“weight-bearing,” fixation,” and “post-operative fixations.” Mesh terms were used when applicable. Wild cards and operators
including “AND”, “OR”, and “NOT” were used when necessary to fine-tune the
research.
The
search results were screened independently by two researchers. Study selection
was based on the eligibility criteria. Exclusion of the study relied first on
the paper’s title then the abstract and followed by full-text screening. The
bibliographic references of the included studies were also manually screened to
find any other eligible studies that may have been missed from previous stages.
Data were extracted and
collected in an electronic spreadsheet for further processing. The extracted
data included the demographic information, age, sex, type of pelvic fracture,
the weight-bearing regimen, the duration of follow-up and weight-bearing, and the
reported results after the application of the weight-bearing regimen whether in
a score format or descriptive discourse. In case of disagreement between the two researchers,
a third researcher acted to resolve any disagreements between the other two researchers.
Quality Assessment
Data Extraction
Data
was obtained from texts and tables, and supplementary data. We focused on the
outcomes of the application of weight-bearing post-fixation of pelvic injury.
Results
Study selection
Strict research was conducted on the pre-set databases using
the keywords, the time limitations, and the article language to minimize the
number of collected articles. Primarily, database research generated 485
articles out of which 73 were duplicates. The records were examined by title and
abstract leading to the exclusion of 393 leaving 19 articles for retrieval.
Four files were not retrieved and only 15 articles were assessed for
eligibility. After reviewing the whole article, nine articles were excluded
because they were not studying pelvic fracture. Finally, 6 articles were
included in the review (Figure 1).
Study characteristics
The characterization of the eligible papers were summarized in Table 1. Five studies adopted the retrospective research design and one study was a randomized controlled trial (RCT). The RCT study was presented with two sets of data. The 6 retrospective studies enrolled 239 patients. In one study, the number of male and female participants could not be retrieved. The number of males in the remaining 5 articles (n=198) was 127 and the females were 71 participants. Tile (n=4) and Young and Burgess (n=2) classifications were used in 5 studies. The pelvic fracture was classified into acetabular and pelvic fractures in one study. All participants had undergone internal fixations with different procedures.
Risk of Bias
Primary outcomes
Pain
The pain was assessed differently in 4 articles (5 datasets)
only. One study used pain control metrics including the need for paracetamol
and opioids (Moussa et al., 2022). In the first dataset (anteroposterior-reduction),
the pain control metric showed 50% use for both paracetamol and opioids
respectively. In the second dataset (posterior reduction), the pain control
metric was 60% and 40% for paracetamol and opioids respectively.
The second study used Majeed scores that includes pain
assessment, 30 points (Wang et al., 2022). The study concluded a significant
reduction of pain means of the Visual Analogue scale VAS score from 7:47 ± 1:54
pre-operatively to 4:06 ± 1:32 post-operatively.
The third study used the pain VAS score to assess pain as well as the need for analgesics (Benhenneda et al., 2022). Pain mean VAS scores improved from 4.1±0.63 preoperatively to 0.9 ±0.25 postoperatively with a significant difference (P<0.0001). The mean dose of morphine consumption for pain was reduced from 5.7± 0.76 mg/d (preoperatively) to 1.6±1.09 mg/d (postoperatively). The mean dose of paracetamol consumption was reduced from 2.2±0.59 g/d (preoperatively) to 1.3±0.40 g/d (postoperatively) with no significant difference (P > 0.05). The fourth study used the percentage (Kezunovic & Bulatovic, 2019). The percentage of patients with pain was 19% (n=41).
Quality of life
The quality of life was not measured directly in any study. However, 2 studies provided data that could reflect the quality of life. The first study used the Majeed score (Majeed, 1989) as an assessment tool for evaluating the clinical and functional outcomes including pain (30 points), standing (36 points), sitting (10 points), sexual function (4 points), and walking (20 points). The excellent and good scores were 87.5% (Wang et al., 2022).
The second study utilized a set of data to analyze the
clinical and functional outcomes (Kezunovic & Bulatovic, 2019) including pain
(19%), activities (87%), range of motion (63%), and power (94%) according to
the Modified Merle d'Aubigné and Postel scoring system (Øvre et al., 2005).
Secondary outcomes
post-operative weight-bearing protocols
All six studies allowed early weight bearing with different protocols. One study allowed full weight bearing in 22 cases (Wang et al., 2022). Three studies allowed immediate weight bearing as tolerated (Poole et al., 2022; Kankanalu et al., 2021; Benhenneda et al., 2022). Another study allowed partially assisted mobilization for 6 months (Moussa et al., 2022). One study adopted early mobilization without providing details (Kezunovic & Bulatovic, 2019).
Discussion
The context of
the study
The current study reviewed the outcomes
of pain and quality of life in patients with post-fixation Tile type-B pelvic
fractures (rotationally unstable but vertically stable pelvic fractures)
who were allowed to early weight-bearing. The review of the literature revealed
that pain was assessed differently across the studies. Generally, early
weight-bearing in these subsets of patients showed marked improvement in pain
scores irrespective of the assessment tools. Moreover, the need for analgesia
postoperatively was markedly reduced. The quality of life was not directly
measured in the retrieved studies. However, other tools including Majeed (Majeed,
1989) and Merle d'Aubigné and Postel scoring were used to
assess the clinical and functional outcomes that can reflect indirectly the
quality of life. Based on these tools, the clinical and functional outcomes
showed marked improvement in patients who were allowed to have early
weight-bearing. The early weight-bearing regimens were variable among the
studies as well as the corresponding pelvic fixation operation.
Agreement and
disagreement with the literature
Concerning pain reduction, recent systematic reviews
concluded that pain was not used as an assessment parameter to evaluate early
weight-bearing post-fixation of pelvic fracture (Murena et al., 2021) (Rickman
et al., 2019). One systematic review stated that pain was used as a non-validated
clinical outcome measure with no further details (Rickman et al., 2019). On the
contrary, according to the results of this review, the pain was the major
outcome in the included studies with positive results. Moreover, analgesic
requirement rates were considered as an additional parameter to the standard
pain scale.
The quality of life was not considered directly in
literature considering early weight-bearing post-fixation of pelvic fracture.
However, Richman and colleagues (2019) reported that the clinical and
functional outcomes were measured using the Majeed (Majeed, 1989) or the modified
Lindahl version (Lindahl et al., 1999) in 19.7% (n=24) of the eligibly reviewed
studies while only 8.2% (n=10) of the studies used SF-36 score that measures
the health-related quality of life. The outcome of these measures was promising
for early weight-bearing (Rickman et al., 2019). In addition, clinical and
functional outcomes were assessed with a modified d’Aubignè Score and Short
Musculoskeletal Function Assessment yielding excellent results (Kazemi &
Archdeacon, 2012). In this review, the Majeed score (Majeed, 1989) and Modified
Merle d'Aubigné and Postel scoring system (Øvre et al., 2005) were utilized. In
agreement with the literature, the clinical and functional outcomes yielded
good results.
This study was comparable to the literature regarding the
use of different weight-bearing regimens. However, the comparison between the
different weight-bearing regimen protocols was not conducted throughout the literature
from the inception of the data based up to the time of conducting this study
(Murena et al., 2021) (Rickman et al., 2019). Herein, the different
weight-regimen protocols were stated without comparison.
It is worth noting that a few number of studies had been
added since the older review studies were published about early weight-bearing
after post-fixation of unstable pelvic fracture (Murena et al., 2021) (Rickman
et al., 2019). Early weight-bearing decision-making is influenced by several
factors such as fracture type, osteosynthesis, concurrent traumas, concurrent
diseases, and implant problems.(Gortler et al., 2018; Hernandez
et al., 2012).
The fear of the loss of reduction, fracture displacement, and poor
post-fixation outcomes is the main reason for the reluctance of orthopedic
surgeons to encourage early weight-bearing (Seo et al., 2020). Moreover, if there is a
substantial probability of surgical failure in one group, an ethical concern arises,
thus preventing patients’ randomization (Rickman et al., 2019).
Strengths and
limitations
The findings of this study came from a sizable sample of
patients that were used to draw these conclusions. Furthermore, to the
knowledge of the author, this is the only study that addressed the pain and the
quality of life (clinical and functional assessment) as the primary outcome of
early weight-bearing post-fixation of pelvic fracture Tile type-B.
The main limitation of this review is that there is no
prospective or comparative cohort study. The studies conducted within the
timeframe of the study were retrospective. The only included RCT compared the
outcomes of two surgical approaches not early weight-bearing against late
weight-bearing. Therefore, direct evidence cannot be delineated to help decision-making
by the treating surgeon.
implementation
of the study
The encouraging findings from this review should motivate
further research to precisely identify the rationale and limitations of early
weight-bearing in patients with rotationally unstable but vertically stable
pelvic fractures. The recognition of the intrinsic stability of the pelvic
fracture, the appropriate fixation technique, and the associated morbidities should
be the basis for the decision of early weight-bearing of post-fixation of
pelvic fracture.
Conclusion
Early weight-bearing has many benefits in the context of Tile
type-B pelvic fracture fixation. Reduction of pain and the dose of analgesic medications
are the promising outcome. Moreover, the functional and clinical outcomes
showed marked improvement as well. In addition,
Early weight-bearing after Tile B pelvic fixation has the
potential to protect patients from bone and muscle loss, joint stiffness, and
early recovery with a short hospital stay. Therefore, early weight-bearing was
proposed to be advantageous in cases of stable and partially unstable pelvic
fractures as well as acetabular fractures. However, the evidence-based protocol
is a challenge. Further research is needed to delineate the appropriate early
weight-bearing protocol corresponding to the type of pelvic fixation operation.
Prospective and cohort studies are recommended for early weight-bearing
decision-making.
References
Ayoung-Chee, P., McIntyre, L., Ebel,
B. E., Mack, C. D., McCormick, W., & Maier, R. V. (2014). Long-term
outcomes of ground-level falls in the elderly. The Journal of Trauma and
Acute Care Surgery, 76(2), 498–503; discussion 503.
https://doi.org/10.1097/TA.0000000000000102
Benhenneda, R., Letissier, H., Dubrana, F., & Di
Francia, R. (2022). Immediate
full weight bearing after pelvic percutaneous fixation by screw for simple
acetabular and pelvic ring fractures in patients older than sixty five years. International
Orthopaedics, 46(10), 2413–2421. https://doi.org/10.1007/s00264-022-05504-z
Bruce,
B., Reilly, M., & Sims, S. (2011). OTA highlight paper predicting future
displacement of nonoperatively managed lateral compression sacral fractures:
Can it be done? Journal of Orthopaedic Trauma, 25(9), 523–527.
https://doi.org/10.1097/BOT.0b013e3181f8be33
Court-Brown,
C. M., & Caesar, B. (2006). Epidemiology of adult fractures: A review. Injury,
37(8), 691–697. https://doi.org/10.1016/j.injury.2006.04.130
Dwyer,
E. P., & Moed, B. R. (2019). Venous thromboembolism after hospital
discharge in pelvic and acetabular fracture patients treated operatively. Journal
of Orthopaedic Surgery (Hong Kong), 27(1), 2309499019832815.
https://doi.org/10.1177/2309499019832815
Eickhoff,
A. M., Cintean, R., Fiedler, C., Gebhard, F., Schütze, K., & Richter, P. H.
(2022). Analysis of partial weight bearing after surgical treatment in patients
with injuries of the lower extremity. Archives of Orthopaedic and Trauma
Surgery, 142(1), 77–81. https://doi.org/10.1007/s00402-020-03588-z
Gill,
J. R., Murphy, C., Quansah, B., & Carrothers, A. (2017). Management of the
open book APC II pelvis: Survey results from pelvic and acetabular surgeons in
the United Kingdom. Journal of Orthopaedics, 14(4), 530–536.
https://doi.org/10.1016/j.jor.2017.08.004
Gortler,
H., Rusyn, J., Godbout, C., Chahal, J., Schemitsch, E. H., & Nauth, A.
(2018). Diabetes and Healing Outcomes in Lower Extremity Fractures: A
Systematic Review. Injury, 49(2), 177–183.
https://doi.org/10.1016/j.injury.2017.11.006
Green,
S., Higgins, P., alderson, P., Clarke, M., Mulrow, D. C., & Oxaman. (2011).
Cochrane Handbook: Cochrane Review: Ch 8: Assessing risk of bias in included
studies. In Cochrane Handbook for: Systematic Reviews of Interventions
(Vol. 6, pp. 3–10).
Hernandez, R. K., Do, T. P., Critchlow, C. W., Dent, R.
E., & Jick, S. S. (2012). Patient-related
risk factors for fracture-healing complications in the United Kingdom General
Practice Research Database. Acta Orthopaedica, 83(6), 653–660.
https://doi.org/10.3109/17453674.2012.747054
Herteleer,
M., Dejaeger, M., Nijs, S., Hoekstra, H., & Laurent, M. R. (2021).
Epidemiology and secular trends of pelvic fractures in Belgium: A
retrospective, population-based, nationwide observational study. Bone, 153,
116141. https://doi.org/10.1016/j.bone.2021.116141
Higgins, J. P. T. (2003). Measuring inconsistency in meta-analyses. BMJ, 327(7414),
557–560. https://doi.org/10.1136/bmj.327.7414.557
Kalmet,
P. H. S., Meys, G., V Horn, Y. Y., Evers, S. M. A. A., Seelen, H. A. M., Hustinx,
P., Janzing, H., Vd Veen, A., Jaspars, C., Sintenie, J. B., Blokhuis, T. J.,
Poeze, M., & Brink, P. R. G. (2018). Permissive weight bearing in trauma
patients with fracture of the lower extremities: Prospective multicenter
comparative cohort study. BMC Surgery, 18(1), 8.
https://doi.org/10.1186/s12893-018-0341-3
Kankanalu,
P., Orfanos, G., Dwyer, J., Lim, J., & Youssef, B. (2021). Can locking
plate fixation of symphyseal disruptions allow early weight bearing? Injury, 52(10),
2725–2729. https://doi.org/10.1016/j.injury.2020.02.094
Kim, J. H., Lim, H., Kim, H. M., & Lim, J. A. (2021).
Intraoperative
development of pulmonary thromboembolism in a bedridden patient owing to a
pelvic bone fracture with negative preoperative computed tomography pulmonary
angiographic findings: A case report. Medicine, 100(29), e26658.
https://doi.org/10.1097/MD.0000000000026658
Kubiak,
E. N., Beebe, M. J., North, K., Hitchcock, R., & Potter, M. Q. (2013).
Early Weight Bearing After Lower Extremity Fractures in Adults: Journal of
the American Academy of Orthopaedic Surgeons, 21(12), 727–738.
https://doi.org/10.5435/JAAOS-21-12-727
Langford,
J. R., Burgess, A. R., Liporace, F. A., & Haidukewych, G. J. (2013). Pelvic
fractures: Part 2. Contemporary indications and techniques for definitive
surgical management. The Journal of the American Academy of Orthopaedic
Surgeons, 21(8), 458–468. https://doi.org/10.5435/JAAOS-21-08-458
Lee, K.
H., Kim, J. Y., Yim, S. J., Moon, D. H., Choi, G. H., & Moon, K. H. (2014).
Incidence and risk factors of subsequent hip fractures in Korea: Multicenter
study. Journal of Korean Medical Science, 29(7), 992–994.
https://doi.org/10.3346/jkms.2014.29.7.992
Lundin,
N., Huttunen, T. T., Berg, H. E., Marcano, A., Felländer-Tsai, L., &
Enocson, A. (2021). Increasing incidence of pelvic and acetabular fractures. A
nationwide study of 87,308 fractures over a 16-year period in Sweden. Injury,
52(6), 1410–1417. https://doi.org/10.1016/j.injury.2021.03.013
Melhem,
E., Riouallon, G., Habboubi, K., Gabbas, M., & Jouffroy, P. (2020).
Epidemiology of pelvic and acetabular fractures in France. Orthopaedics
& Traumatology, Surgery & Research: OTSR, 106(5), 831–839.
https://doi.org/10.1016/j.otsr.2019.11.019
Miyamoto, R. G., Kaplan, K. M., Levine, B. R., Egol, K.
A., & Zuckerman, J. D. (2008). Surgical
management of hip fractures: An evidence-based review of the literature. I:
femoral neck fractures. The Journal of the American Academy of Orthopaedic
Surgeons, 16(10), 596–607.
https://doi.org/10.5435/00124635-200810000-00005
Moher,
D., Liberati, A., Tetzlaff, J., Altman, D. G., & The PRISMA Group. (2009).
Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA
Statement. PLoS Medicine, 6(7), e1000097.
https://doi.org/10.1371/journal.pmed.1000097
Murena, L., Canton, G., Hoxhaj, B., Sborgia, A., Fattori,
R., Gulli, S., & Vaienti, E. (2021). Early
weight bearing in acetabular and pelvic fractures. Acta Bio-Medica: Atenei
Parmensis, 92(4), e2021236. https://doi.org/10.23750/abm.v92i4.10787
Nelson,
J. T., Coleman, J. R., Carmichael, H., Mauffrey, C., Vintimilla, D. R.,
Samuels, J. M., Sauaia, A., & Moore, E. E. (2020). High Rate of
Fibrinolytic Shutdown and Venous Thromboembolism in Patients With Severe Pelvic
Fracture. The Journal of Surgical Research, 246, 182–189.
https://doi.org/10.1016/j.jss.2019.09.012
Önsten,
I., Berzins, A., Shott, S., & Sumner, D. R. (2001). Accuracy and precision
of radiostereometric analysis in the measurement of THR femoral component
translations: Human and canine in vitro models. Journal of Orthopaedic
Research, 19(6), 1162–1167.
https://doi.org/10.1016/S0736-0266(01)00039-0
Paulsson,
M., Ekholm, C., Jonsson, E., Geijer, M., & Rolfson, O. (2021). Immediate
Full Weight-Bearing Versus Partial Weight-Bearing After Plate Fixation of
Distal Femur Fractures in Elderly Patients. A Randomized Controlled Trial. Geriatric
Orthopaedic Surgery & Rehabilitation, 12, 21514593211055890.
https://doi.org/10.1177/21514593211055889
Poole,
W. E. C., Neilly, D. W., & Rickman, M. S. (2022). Is unrestricted weight
bearing immediately after fixation of rotationally unstable pelvic fractures
safe? BMC Musculoskeletal Disorders, 23(1), 348.
https://doi.org/10.1186/s12891-022-05299-5
Rickman,
M., Link, B.-C., & Solomon, L. B. (2019). Patient Weight-bearing after
Pelvic Fracture Surgery—A Systematic Review of the Literature: What is the
Modern Evidence Base? Strategies in Trauma and Limb Reconstruction, 14(1),
45–52. https://doi.org/10.5005/jp-journals-10080-1414
Rinne, P. P., Laitinen, M. K., Kannus, P., & Mattila,
V. M. (2020). The
incidence of pelvic fractures and related surgery in the Finnish adult
population: A nationwide study of 33,469 patients between 1997 and 2014. Acta
Orthopaedica, 91(5), 587–592. https://doi.org/10.1080/17453674.2020.1771827
Roberts,
K. C., Brox, W. T., Jevsevar, D. S., & Sevarino, K. (2015). Management of
Hip Fractures in the Elderly. JAAOS - Journal of the American Academy of
Orthopaedic Surgeons, 23(2), 131–137. https://doi.org/10.5435/JAAOS-D-14-00432
Seo,
H., Lee, G. J., Shon, H.-C., Kong, H. H., Oh, M., Cho, H., & Lee, C. J.
(2020). Factors Affecting Compliance With Weight-Bearing Restriction and the
Amount of Weight-Bearing in the Elderly With Femur or Pelvic Fractures. Annals
of Rehabilitation Medicine, 44(2), 109–116.
https://doi.org/10.5535/arm.2020.44.2.109
Sulmasy,
D. P. (2019). Ethics and Evidence. The Journal of Clinical Ethics, 30(1),
56–66.
Tile,
M. (1996). Acute Pelvic Fractures: I. Causation and Classification. JAAOS -
Journal of the American Academy of Orthopaedic Surgeons, 4(3),
143–151.
Tile, M., & Pennal, G. F. (1980). Pelvic disruption: Principles of
management. Clinical Orthopaedics and Related Research, 151,
56–64.
Xiong,
B., Yang, P., Lin, T., Xu, J., Xie, Y., Guo, Y., Liu, C., Zhou, Qi., Lai, Q.,
He, W., Wei, Q., & Zhang, Q. (2022). Changes in hip joint contact stress
during a gait cycle based on the individualized modeling method of
“gait-musculoskeletal system-finite element.” Journal of Orthopaedic Surgery
and Research, 17(1), 267. https://doi.org/10.1186/s13018-022-03094-5
Yoshida,
H., Faust, A., Wilckens, J., Kitagawa, M., Fetto, J., & Chao, E. Y.-S.
(2006). Three-dimensional dynamic hip contact area and pressure distribution
during activities of daily living. Journal of Biomechanics, 39(11),
1996–2004. https://doi.org/10.1016/j.jbiomech.2005.06.026
Yoshihara,
H., & Yoneoka, D. (2014). Demographic epidemiology of unstable pelvic
fracture in the United States from 2000 to 2009: Trends and in-hospital mortality.
The Journal of Trauma and Acute Care Surgery, 76(2), 380–385.
https://doi.org/10.1097/TA.0b013e3182ab0cde
Young,
J. W., Burgess, A. R., Brumback, R. J., & Poka, A. (1986). Pelvic
fractures: Value of plain radiography in early assessment and management. Radiology,
160(2), 445–451. https://doi.org/10.1148/radiology.160.2.3726125
Figures
Figure 1: PRISMA
flow diagram.
Tables
Table 1:
the characterization of the eligible papers



Comments
Post a Comment